Osteochondrosis is a chronic disease in which the disease, changes occur in the vertebrae and situated between them intervertebral disks. Depending on the lesion of the spine are: the cervical osteochondrosis, osteochondrosis of the thoracic and osteochondrosis of the lumbar region of the spine. For the diagnosis of osteochondrosis of the spine need radiography, and in case of complications (for example, herniated disc) - spinal MRI. In the treatment of osteoarthritis of the spine, along with the medical methods are widely used, reflexology, massage, manual therapies, physiotherapy and exercise therapy.
Etiology and pathogenesis
In different degrees, osteochondrosis occurs in older people and is one of the aging process. Sooner or later in the intervertebral disc can produce atrophic changes, however, of injury, disease and the different overloads of the spine contribute to the earlier onset of osteoarthritis. The most common osteochondrosis of the cervical and degenerative disc disease of the lumbar spine.
There are about 10 theories of degenerative disc disease: vascular, hormonal, mechanical, genetic, infectious-allergic and other. But none of them gives a complete explanation of what is happening in the spine changes, but they are complementary.
It is believed that the main point in the appearance of osteoarthritis is the constant overload of the vertebral motor segment, which consists of two vertebrae adjacent. This overload can result from the patterns of movement — posture, the individual way of sitting and walking. Incorrect posture, sitting in a wrong posture, walking with an uneven spine cause extra strain on discs, ligaments and muscles of the spine. The process can be aggravated due to the peculiarities of the structure of the spine and the failure of trophic its tissues due to hereditary factors. More often, the defects in the structure occur in the cervical spine and lead to vascular disorders and the first signs of degenerative disc disease of the cervical spine.
The appearance of osteochondrosis of the lumbar region, often associated with the overload on the stoop, and lift weights. A healthy intervertebral disc can withstand a considerable loads due to the hydrophilicity located in the center of the nucleus pulposus. The kernel contains a lot of water and fluids, as you know, a little compressed. The breakdown of a healthy intervertebral disc can occur when the compression force of more than 500 kg, while changed as a result of degenerative disc disease the disc breaks when the compression force of 200 kg. Load of 200 kg experiences a lumbar spine of a person who weighs 70 kg, when kept at 15 kilos of cargo on the position of the torso forward at 200. A great pressure because of the small size of the nucleus pulposus. When the inclination increases to 700, the load on intervertebral discs is 489 kg. So, often the first clinical manifestation of osteochondrosis of the lumbar region of the spine occur during or after heavy work, the realization of the tasks of the home, weeding the garden, etc.
The destruction of the connective tissue of the ring fibrous of the disc, ligaments and capsules of the joints causes a reaction of the immune system and the development of aseptic inflammation with the inflammation of the joints and the surrounding tissues. Due to the displacement of the vertebral body is stretching of the capsule of the joints, and changed the intervertebral disc is not so firmly locks the body of the vertebrae adjacent. Format of the instability of the spinal segment. Due to the instability of the possible infringement of the nerve roots of the spinal nerve with the development of the syndrome root. Osteochondrosis of the cervical spine often occurs in the curves of the head, osteochondrosis of the lumbar spine during trunk flexion. The formation of the functional unit of the vertebral motor segment. It is due to the compensatory contraction of vertebrate muscles.
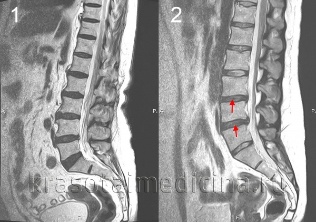
A herniated disc occurs when the disc moves backward, there is a rupture of the posterior ligament longitudinal and bulging of the disc into the spinal canal. If the spinal canal is pressing the kernel from the disk, this is called a ruptured hernia. The severity and duration of pain associated with a hernia is much more than the unexploded. A herniated disc may cause radicular or syndrome of compression of the spinal cord.
When osteochondrosis occurs, the expansion of the bone with formation of osteophytes — bony growths in the body and the vertebrae. Osteophytes can also cause compression of the spinal cord or cause the development of the syndrome root.
The symptoms of osteochondrosis
The main symptom of osteochondrosis is pain. The pain can be sharp with high intensity, which increases with the slightest movement in the segment affected and, therefore, forces the patient to take a forced situation. Thus, in osteochondrosis of the cervical spine, the patient keeps the head in the least painful position, and cannot rotate, osteochondrosis of the thoracic pain is even worse with a deep breath, and osteochondrosis of the lumbar region of the patient is difficult to sit, stand and walk. As a pain syndrome is characteristic of the compression of the nerve root of the spinal nerve.
Approximately 80% of cases, there is dull pain constant in nature and of moderate intensity. In these cases, during the examination, the doctor needs to differentiate between the manifestations of osteochondrosis of the spine, of myositis in the musculature of the back. Dull pain in osteochondrosis is caused by excessive tension of the muscles that support the affected vertebral motor segment, inflammatory changes or significant stretching of the intervertebral disc. Patients with this pain syndrome forced position is missing, but revealed limitation of movement and physical activity. Patients with osteochondrosis of the cervical spine, avoid sharp turns and tilts the head, osteochondrosis of the lumbar - slowly sit down and get up, avoid the bending of the trunk.
Complications of spinal osteochondrosis
Complications of degenerative disc disease associated with disc hernia. These include compression of the spinal cord, which is characterized by numbness, weakness of certain muscle groups of the limbs (depending on the compression level), which leads to the appearance of the paresis, muscle atrophy, changes in tendon reflexes, disturbances of urination and defecation. A herniated Disc can cause compression of the artery feeding the spinal cord, with the formation of areas ischemic (infarction of the spinal cord), with the loss of nerve cells. This is manifested by the appearance of a deficit neurological (violation of movements, loss of sensibility, trophic disorders), appropriate to the level and extent of the ischemia.
Diagnosis of osteochondrosis
The diagnosis of osteochondrosis is directed by the neurologist or spine. In the initial phase of producing x-rays of the spine in 2 projections. If necessary, you can do a survey of single segment vertebral and shoot additional images. For the diagnosis of intervertebral hernia, the evaluation of the spinal cord and to detect complications of degenerative disc disease using magnetic resonance imaging (MRI of spine). Great role of magnetic RESONANCE imaging in the differential diagnosis of osteochondrosis and other diseases of the spine: tuberculous spondylitis, osteomyelitis, tumors, ankylosing spondylitis, rheumatism, infections. Sometimes complicated cases of degenerative disc disease of the cervical spine exclusion is necessary syringomyelia. In some cases, the inability of magnetic RESONANCE myelography is shown.
Sighting study the affected intervertebral disc is possible with the discography. Electrophysiological studies are used to determine the extent and location of the lesions of the nervous system pathways, and the monitoring of their recovery during therapy.
Treatment of osteochondrosis
In the acute period are shown in the rest of the affected vertebral motor segment. With this goal in osteochondrosis of the cervical spine is used, fixation by means of collar Trench, osteochondrosis of the lumbar region of the bed. The fixation of the cervical osteochondrosis with instability of the spinal segment.
Drug therapy for degenerative disk disease use of nonsteroidal anti-inflammatory drugs (Nsaids): diclofenac, nimesulide, lornoxicam, meloxicam. With intense pain syndrome shows analgesics, for example, the Central analgesic action of flupirtine. To alleviate muscle tension and the use of muscle relaxants — tolperisone, tizanidine. In some cases, the use of appropriate anticonvulsants - carbamazepine, gabapentin; antidepressants, among which preferably inhibitors of serotonin reuptake (sertraline, paroxetine).
On the incidence of the syndrome radicular patient sample of inpatient treatment. Perhaps a local injection of glucocorticoid, in the treatment against edema, the use of traction. In the treatment of osteoarthritis are widely used in physiotherapy, reflexology, massage, physiotherapy. The use of manual therapy requires strict adherence to the techniques of execution and special care in the treatment of degenerative disc disease of the cervical spine.
The surgery is shown mainly with significant compression of the spinal cord. It consists of the removal of the herniated disc and decompression of the spinal canal. It is possible to perform microdiscectomy and laser disc reconstruction, replacement of the affected disc implant and the stabilization of the spinal column segment.












































